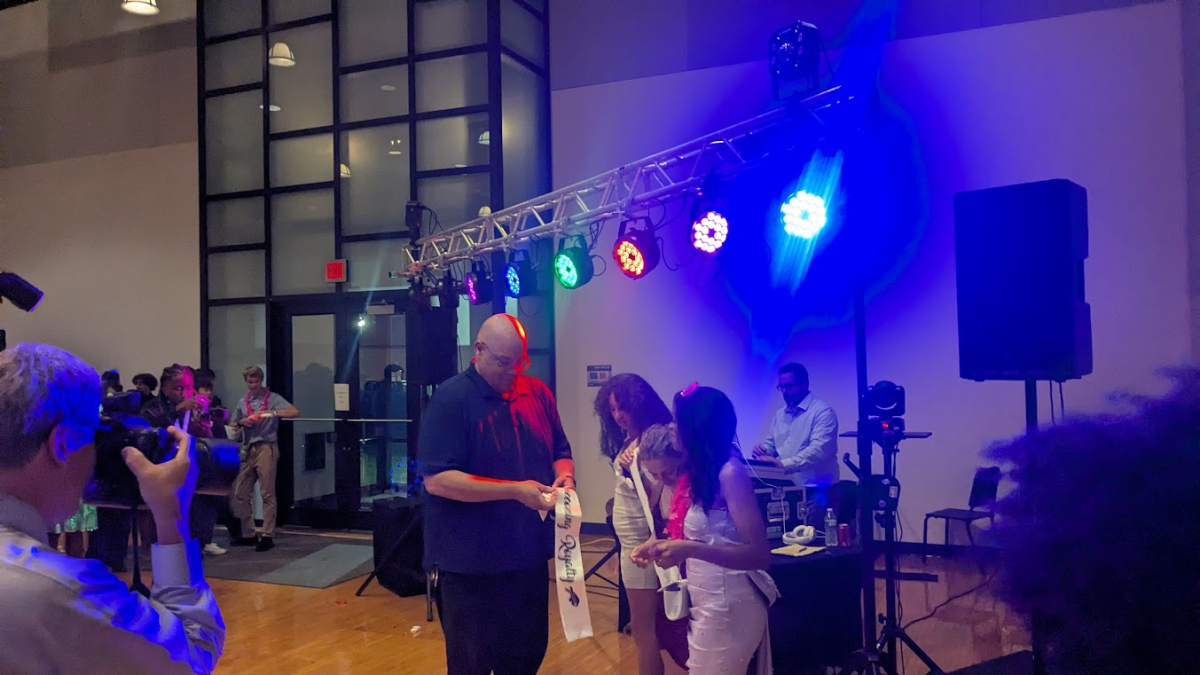
A recovery speaker visited Lauren Bambrick’s health class on April 23 to describe his journey of overcoming addiction.
SAY/SADD Counselor Cindy Toncler emphasized the importance of the discussion.
“It’s a powerful thing for a young person to hear somebody who’s not that much older than they are, who has been through a tough time,” she said.
Due to privacy reasons, the speaker’s name could not be shared, but Bambrick explained that he was a young man in his early 20s who grew up in the area, and who had been in recovery for some time.
“He provided his story and allowed for a question-and-answer session with the students in our health classes,” she said.
Sophomore Eilah Epstein recounted what the speaker had shared about his story.
“He said that he tried marijuana with some people and that once he started he kept looking for more,” she said. “He stopped caring about wrestling—even though he was really good at it—and eventually stopped going to class. He shared that he would wake up each day excited just so he could use drugs.”
Once he started using marijuana and alcohol, his addiction spiraled out of control and advanced quickly. He did not gain access to opioids and was glad that he never did because he said his life would have been put in major jeopardy.
Bambrick brought in the speaker as part of her comprehensive unit on substance abuse.
“We talk about the risk factors, protective factors, impacts, consequences and recovery resources to help individuals who suffer from substance abuse,” she said.
By educating students on these critical issues, her class reflects the reality that drug abuse is not just a personal issue but a complex and widespread problem that affects millions across all age groups and demographics.
90% of these opioid-related deaths involved the use of synthetic opioids such as Fentanyl, which are opioids produced in labs, making them easily accessible and even more potent due to the risk of being mixed with other drugs.
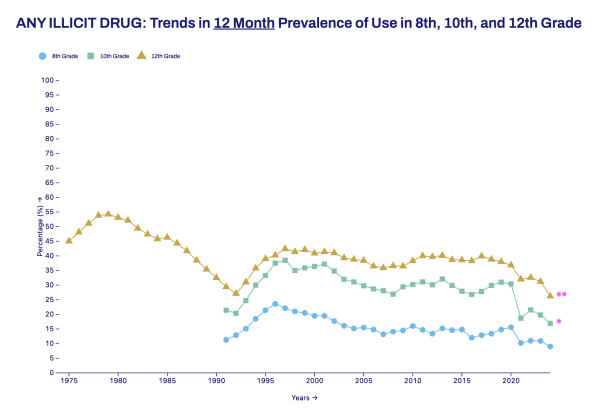
While these numbers highlight the seriousness of drug abuse among the general population, recent trends among adolescents tell a more hopeful story.
According to the 2024 Monitoring the Future Survey, funded by the National Institutes of Health, substance use among teens has remained at low levels for the fourth year in a row.
Since a sharp decline during the COVID-19 pandemic, reported use of drugs and substances such as alcohol, nicotine and cannabis has either stayed low or continued to decrease among eighth, tenth and twelfth graders.
Still, these findings should not overshadow the urgency of the ongoing opioid crisis, which led to over 700,000 overdoses between 1999 and 2022.
Sarah Huntington, a representative of the Pepper Pike treatment facility New Directions, confirmed that fentanyl use in particular has become more visible among teens.
“More teens seem to be using it, or at least admitting they are,” she said. “Fentanyl use is much more openly acknowledged now than it was before.”
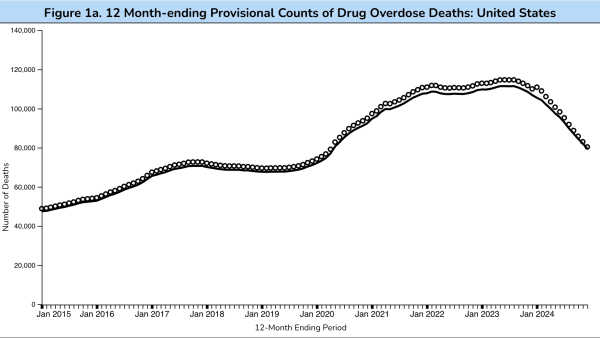
And while data from the Centers for Disease Control and Prevention shows a drop of more than 26% in fentanyl-related deaths since the peak in June 2023, Huntington made it clear that the crisis is far from over.
“It’s still a major concern,” she said. “While overdose deaths might have slightly decreased according to the latest data, they remain high. Fentanyl continues to be a significant cause of death.”
Perhaps most troubling, she added, is a lack of full awareness about the severity of the danger.
“[People are] not nearly [aware] enough,” she said. “People have a general idea that opioids are dangerous, but they don’t fully grasp how serious and deadly the situation really is.”
While the consequences are severe for people of all ages, and although drug use in general is down among teens, teenagers remain particularly vulnerable. In 2022, drug overdose killed an average of 22 high school age adolescents each week in the United States.
Given these alarming statistics, it’s important to understand the factors that put teens at greater risk.
It’s widely known that family history, mental conditions, peer pressure and environment are some of the common contributing factors to substance abuse.
Toncler revealed some of the major factors she had noticed throughout her experience as a counselor.
“Teenagers are more likely to experiment if they have easy access, especially with the laws changing with marijuana, for example,” she said. “In our state, because it’s now legal recreationally, attitudes about marijuana have shifted, and even though it’s not legal for teenagers, the general perception is that it’s not as bad as it once seemed.”
Although many teens don’t view marijuana as dangerous, Toncler emphasized that teenagers are experiencing major consequences due to its harmful effects.
“With the high TAC (Total Active Cannabinoids) levels in marijuana nowadays, young people are having psychotic episodes and ending up in the emergency room because they’re hallucinating,” she said.
Toncler also explained that the perceptions of substances in one’s social circle can impact experimentation with drugs.
“Teenagers may be more likely to experiment if the perception with the people closest to them, their friends and their family, is more laid back, and if they perceive that there is not really a major consequence,” she said.
Aside from perception and easy access, Toncler clarified other conditions that teenagers face that contribute to them trying substances.
She emphasized how the prevalence of anxiety nowadays affects substance abuse as well.
“With the added pressures of being a teenager… we have a lot more people with anxiety than ever before,” Toncler said. “Grabbing onto things that help them to [temporarily] not feel that discomfort, such as finding a drug that does that for them, makes them more likely to turn to such things.”
To combat this, Toncler remarked that if adults communicate clearly that it’s not okay for teenagers to abuse substances, then the teens are less likely to participate.
Echoing Toncler’s perspective, Huntington added further insight into how a variety of influences–especially from a teen’s immediate environment–can contribute to experimentation.
“What I’ve noticed is a lot of exposure through parents,” said Huntington. “If there is drug use in the house, they’re more likely to experiment–or if a close friend’s parents are using–because then they have easy access and exposure.”
She also pointed to media portrayal as a growing concern.
“I think there’s a lot of glorification that goes on right now in the media,” Huntington said. “Shows like Shameless or Euphoria make teens curious. Rather than seeing the negatives, it’s more like, ‘Oh, hey, I wanna try that.’”
Drug abuse has been known to affect a teen’s academic performance, relationships with peers and overall mental health.
Toncler shared the impacts that drug use can have on a person’s life, depending on the stage of abuse.
“If somebody is just experimenting, we might not see any major effects at all, and they might just be fine with school and their relationships,” she said. “If they move into social use, they often still are able to keep [their] life together, but you begin to notice that more of their choices are geared towards substances, such as a shift in their friend group.”
Toncler explained how the effects of substance abuse can escalate.
“Teenagers may lose motivation in activities, and at school, you might begin to notice they are tardy more, and showing up and having less energy,” she said.
Huntington elaborated on how deeply substance abuse can affect a teenager’s life.
“You’re not able to focus any more because you’re high all the time,” she said. “Things that used to mean something to you no longer really do. You might be going through withdrawal, so you’re too sick to do anything.”
She also emphasized the toll on families.
“No parent wants to see their child killing themselves slowly through drug use,” she said. “That causes more arguments at home, more division. Sometimes the teen starts stealing money or drugs from their parents. In the worst cases, CPS [Child Protective Services] or the courts might have to get involved.”
The larger trend of drug abuse has also been reflected in the opioid crisis.
Toncler explained that opioid abuse was most prevalent during the years prior to the COVID-19 pandemic.
One factor in the reduction of use was that it has become harder to get a prescription.
“It used to be that if you had your wisdom teeth removed, your doctor would give you a full bottle of opioids for your pain relief, including teenagers, and there was no deterrent to that,” she said.
Now, given the alarming death rates in relation to opioid abuse and overdose, regulations have been tightened to reduce access to such substances, limiting the ability of medical professionals to prescribe them for pain relief.
For example, according to the Ohio Board of Pharmacy, the state has implemented regulations that limit opioid prescriptions for adults to a seven-day supply for acute pain.
For minors, the initial prescription is limited to a five-day supply, and prescribers must obtain written consent from a parent or guardian before prescribing.
“Because of the [epidemic of opioid deaths], doctors are no longer allowed to prescribe [as many pills at a time],” Toncler said. “Even when people come back from surgery, they are still limited with how many tablets are available to them, so you’re seeing [fewer] teenagers able to abuse opioids.”
Toncler also mentioned that pharmaceutical manufacturers have taken steps to prevent abuse.
“Manufacturers changed how they were making the tablets,” she said. “They used to be able to crush them. Now they coat them, meaning it tends to slow down the effects of the medication as people aren’t able to crush it and get more of an immediate high. It’s a way to deter the ability to abuse that type of medication.”
Fortunately, with these prevention factors, Toncler explained how overdoses have started to decrease, but only gradually.
In fact, according to the Ohio Department of Health, in 2023, Ohio experienced a 9% decrease in unintentional drug overdose deaths, marking the second consecutive year of decline.
One of the main contributing factors to this decline in deaths has been a medication called Naloxone, typically given as a nasal spray, which reverses an opioid overdose by attaching to opioid receptors and blocking the effects of other opioids.
Programs like Project DAWN have distributed over 290,000 naloxone kits across the state just in 2023, according to the Begun Center for Violence Prevention Research and Education.
This availability is critical, as naloxone can be life-saving in emergencies, and in cases of opioid overdose where a person’s breathing has slowed or stopped, it can rapidly restore normal breathing.
However, naloxone prescription isn’t common in emergency departments.
A survey of emergency physicians (EPs) published in the Journal of Opioid Management in 2023 found that 65% of residents and 33.3% of attending physicians had never prescribed naloxone despite agreeing it was safe and ethical.
One of the primary barriers identified to prescribing naloxone was the time needed to counsel patients on its use, highlighting the need for interventions to make naloxone distribution more common and effective.
While fentanyl poses a significant ongoing threat, efforts to increase access to naloxone could help mitigate its deadly impact.
At the same time, Huntington emphasized just how present the danger still is, especially with teens.
“Fentanyl is still a huge concern. We’re still seeing overdose deaths, maybe a little less, but it’s still very much out there,” she said. “Some teens now even admit to seeking it out specifically, even knowing how deadly it is.”
The ongoing danger has had a devastating impact on families across the community.
“[We have seen] a lot of death,” she said. “Between parents overdosing and leaving children behind, and children overdosing themselves, the loss is significant.”
Mental health challenges are often tied to substance use, as Huntington observed.
“98 to 99% of the time, there’s a co-occurring mental health disorder like anxiety or depression,” she said. “Sometimes teens use substances to self-medicate, but it often ends up making the conditions worse.”
She added that while marijuana remains the most widely used drug among adolescents, other harder substances are increasingly showing up.
“Cocaine is a big one, and we’re seeing more teens using opiates again,” she said. “Around 2016, fentanyl started appearing in street drugs, and many people tried switching to meth to avoid it–but eventually, even meth got laced with fentanyl. Now, ten years later, some teens and adults actively seek it out despite its dangers.”
In response to the crisis, New Directions has expanded its approach to treatment.
“Our psychiatrist now runs what’s called a MAT program [Medication-Assisted Treatment] for opioid addiction,” she said. “Clients take medication that helps with cravings, which makes them less likely to return to using.”
Huntington also explained the various levels of the treatment process.
“We start with an assessment to see what the person needs,” Huntington said. “From there, we might offer outpatient, intensive outpatient (four days a week with group therapy), or residential treatment. We stay connected with the client through every stage, including community outreach and long-term recovery.”
But even with strong support systems in place, common misconceptions still make it harder to address the issue early.
“One big [misconception] is that experimentation is normal,” Huntington said. “It might start that way, but many parents don’t realize when it shifts into abuse or even addiction. Sometimes they’re just not ready to admit their kid has a problem.”
To anyone who is facing addiction, she offered a simple message:
“If anybody is struggling with substance use or thinks they might have a problem, please reach out,” Huntington said. “We’re a very nonjudgmental facility–we’re here to help.”
Beyond just clinical support, Huntington emphasized the importance of community and follow-through.
“We try to stay with our clients as long as possible,” she said. “Even after they finish residential treatment, we continue with intensive outpatient care and, eventually, outpatient and community outreach. That way, we can maintain that connection and accountability.”
As the opioid crisis and broader substance use issues continue to impact young people, professionals agree on one key factor–early intervention is crucial.
“There are warning signs that parents and schools can look for–changes in friend groups, dropping grades, lack of motivation, mood swings,” Huntington said. “The earlier someone steps in, the more likely that teen can get back on track before it becomes a long-term struggle.”
Education, communication and access to resources remain critical in helping teenagers resist the influence of substance abuse.
Programs at Beachwood and facilities like New Directions continue working hand-in-hand to address substance abuse from all sides.
BHS Students struggling with substance abuse and mental health issues related to addiction have resources available.
Toncler said that students can always meet with her with concerns they may have, in addition to the numerous other staff members in our schools.
“All students have access to meet with me,” she said. “But certainly, there are lots of people here at Beachwood that students can talk to. The staff here, the counselors, the psychologists, and the principal are all really concerned and want young people to overcome and get everything they need to be successful.”
Other sources at the school, including the SAY/SADD club, are striving to clearly address this issue and other problems arising within teens.
Moreover, the ADAMHS Board of Cuyahoga County has a link to a list of resources for people struggling with addiction, in addition to SAMHSA, a national organization that provides a list of general resources regarding substance abuse and mental health services on their website.
Whether through school-based counseling, peer support groups, or treatment centers offering comprehensive care, help is not only available–but encouraged.
“People often think they need to hit rock bottom to get help,” Huntington said. “But the truth is, the sooner you seek support, the better your chances are of recovering and reclaiming your life.”